1. Introduction
Anal warts are neoplastic lesions associated with tropism for squamous epithelial cells and caused by oncogenic and non-oncogenic human papillomavirus (HPV). Condylomata acuminata, the common malignant-associated subset of anal warts, usually appear in reproductive-age individuals. HPV infection is thought to be common, but the majority of lesions remain asymptomatic and undetected, generating surveillance and management challenges. Other anal warts may not be associated with HPV or may represent circumferential, squamous-lined, single or multiple rectal ectopic sebaceous glands and ectopic rectal apocrine glands.
Anal warts can be recognized using clinical criteria, with visual assessment and anoscopic findings being sufficient in most instances. When benign, biopsy is rarely indicated, and imaging is reserved for atypical lesions. Management is guided by lesion characteristics and patient preference. Vaccination against high-risk HPV types is a powerful preventive strategy, and greater awareness of risk factors and HPV transmission may also reduce burden.
2. Etiology and Pathophysiology
Anal warts (condylomata acuminata) are benign neoplasms that occur in the peri-anal or anorectal region due to infection with the human papillomavirus (HPV). Although anal warts usually are asymptomatic, they may be associated with anal pain, itching, bleeding, or discharge. Anal warts have a natural history of spontaneous regression in immunocompetent hosts; however, such regression does not preclude alcoholic hepatitis, re-infection, or the appearance of new anal warts. Anal warts can progress to dystoplasia, anal pre-cancer, or anal cancer.
Anal warts should be differentiated from other anorectal growths that may occur in the same anatomical region. As anal warts are sexually transmitted lesions, they share HIV co-infection risk factors. Smoking, extensive genital or oral condylomatosis, a history of transplant rejection, and pregnancy are also co-factors for persistent infection with HPV related to the development of analwarts. Distinction between the various lesions based on histopathological criteria is pursued. Despite the use of the latter criterion, clear distinction remains impossible in all circumstances. Conversely, condylomata acuminata develop in response to low-risk HPV strains (i.e. HPV 6, 11) and resolve with local treatment.
3. Epidemiology
Anal warts are sexually transmitted lesions caused by specific strains of human papillomavirus (HPV). Their development may be due to infected sexual partners, extragenital sources, or self-inoculation. Anal warts are usually symptomatic but can also remain unnoticed. Certain populations are at increased risk, presentation can vary, and diagnostic surveillance should be tailored to the individual.
Risk factors and events leading to their causation can be synthesized along with sexually transmitted HPV infection, its persistence, population prevalence patterns, and fecal incontinence. Evidence from population-wide studies and groups at increased risk indicate that anal warts predominantly arise in men who have sex with men (MSM)—especially those who are HIV-positive or HIV-negative with other risk factors who are receptive to anal intercourse—and in women with cervical cancer cofactor lesions (cervical pre-cancer and cancer, external genital warts, and laryngeal papillomatosis). Whether they occur in non-MSM men and women is an open question.
Growths in the anal region—whether anal warts or not—can be provisionally separated into condylomata acuminata and other forms. The former are associated with HPV infection and anogenital sexual behavior and are driven by HPV’s notorious capacity for immune evasion. These two characteristics, when combined with the recipient host’s level of immunosuppression and the level of risk taken by whichever partner has those infection sources, together shape the natural history of convergence, emergence, and resolution. Evidence-based clinical guidelines exist for the diagnosis and management of anal warts. Condylomata acuminata are usually symptomatic but may be asymptomatic; nondetection decreases with temporal proximity to the previous sexual intercourse in both men and women.
4. Clinical Presentation and Diagnosis
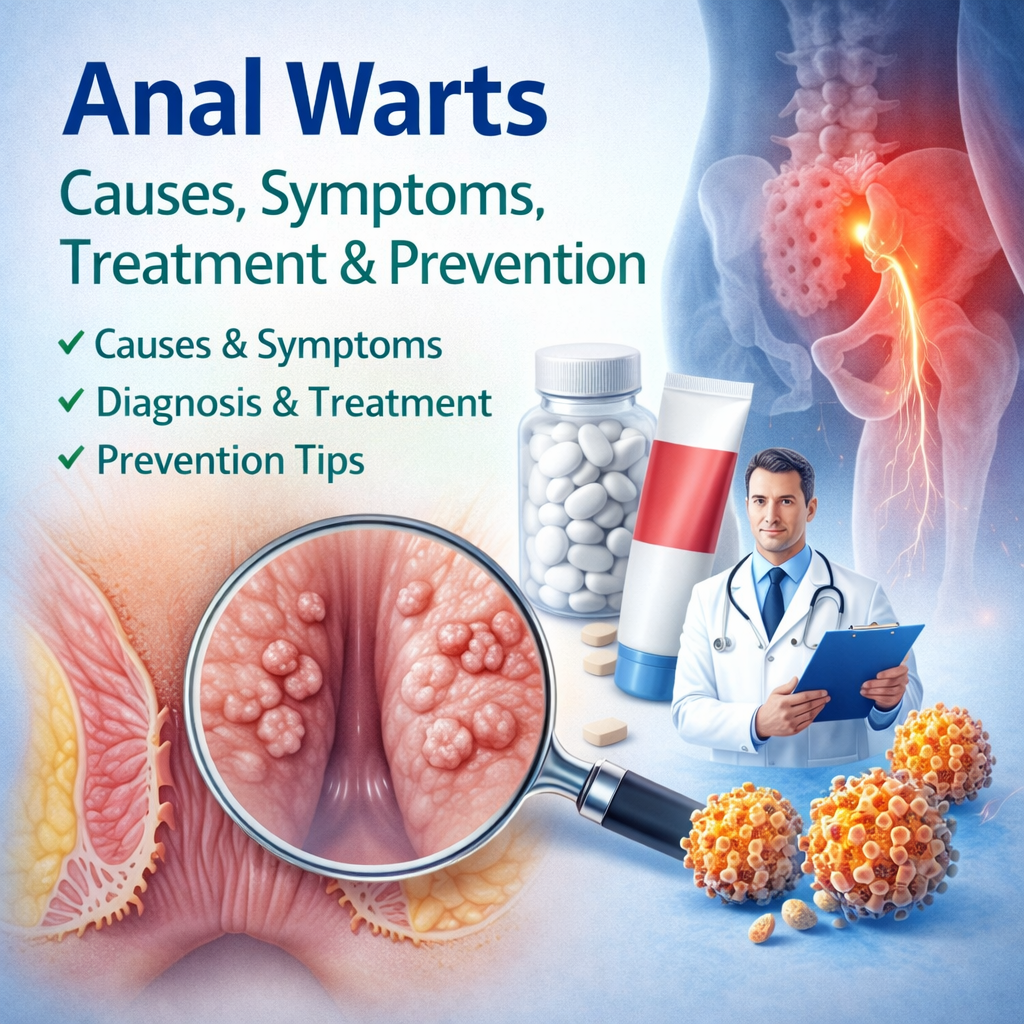
Clinical diagnosis of anal warts is based on characteristic visual features and the observation of these lesions in a typical anatomic location. Anoscopy or coloscopy in the absence of a concomitant anal wart may reveal other lesions. Within atypical cases, histological testing may be necessary to exclude malignancy; lesions not otherwise clinically diagnosed should be considered for biopsy with HPV typing to establish anal cancer risk.
In the typical presentation of anal warts, these growths are found in the perianal area. They appear as raised or slightly elevated lesions, with a smooth surface and a normal color; however, they may also be pigmented, excrescent and prominent, or stellate. When condylomata acuminata are prominent, they may give the anal margin the appearance of a cauliflower and may occlude the anal orifice. Condylomata acuminata are not sensitive, but larger lesions may cause discomfort, itching, or bleeding, especially during defecation.
Less frequently, these growths may occur intrarectally and simulate an infiltrating process. Anoscopy may reveal inner developments behind an unaffected anal margin, inside a normal-appearing anal canal, or in a free anal pit. A colposcopically visible process inside the anal canal but masked by the external opening, an intra-anal process, or located above the anal canal may also be observed.
5. Management and Treatment
Management principles are based on observations that anal warts (cause a) are benign and may self-resolve; (co)-exist asymptomatically in many immunocompetent individuals; have spontaneous regression associated with immune responses; and can be treated effectively yet recurrences are common. Consequently, management consists of removing symptomatic lesions to relieve symptoms, prevent complications, or minimize transmission risk in selected cases.
Decision-making considers a patient’s overall health and prognosis, the extent of warty lesions, and associated HPV-related disease. Importantly, management prioritizes patient safety, a preference for non-surgical modalities, treatment adherence difficulty, and lesion size predictiveness of topical therapies (i.e. smaller lesions respond better), supported by a recent meta-analysis. Although pharmacological therapies are safe and effective, none are superior, and surgery is beneficial mainly for larger lesions. Despite their efficacy, topical agents have low natural-responder rates, especially when applied to multiple lesions. Available procedural therapies are inherently invasive and painful; despite an acceptable safety profile, these have lower cure rates and are prone to recurrence. Operator experience and patient cooperation influence outcomes, whereas the anaesthetic methods employed SERdge whether patients regard surgery as comfort- or pain-driven.
Treatment starts with topical agents unless the patient is immunocompromised or a sensory deficit is present. The decision to use any of the topical treatments depends on their ease of use, with imiquimod being favoured. Response rates are lower in disease other than condylomata acuminata. Recurrences are common, especially in women.